Self-funded Administration
EMI Health has been a partner for groups like yours from day 1, starting with large education groups in Utah in 1935. Our expertise in self-funded administration - and bonus features - make us the best choice for your medical, dental, and vision plan administration.
Cost-saving features
Customizable plans designs. Bonus features that save time and money. Now is the time to celebrate.
-
· Telemed: Unlimited, $0 copay, 24/7/365 access to virtual consultations with board-certified physicians through our partner WellVia for less than $5 PEPM.
-
· Wellness: We combine onsite services and multiple digital resources in our robust wellness program that is included in our medical plans. We even offer options for customizable challenges and rewards.
-
· Pharmacy programs: Through our preferred PBM partner Express Scripts, we offer programs that significantly reduce claims costs for prescription drugs.
-
· Access to top national networks: We have partnered with some of the top names in the industry to make sure your employees have access to participating providers wherever they are in the USA.

Reduce Your Risk
For more than 85 years we have been navigating the healthcare industry and guiding our self-funded groups.
Organizations like yours stay with EMI Health because we use the same claims scrubbing and medical management for our self-funded clients as for our fully-insured clients, translating to you getting the lowest costs for medical services that we can get. We have a high standard for claims processing, leading to a 6.4 day turnaround and overall claims accuracy rate of 99.9%.
An admin fee that has it all
We believe in transparency, so our administrative fee is intentionally inclusive. No hidden fees, no nickel-and-dime practices, and no more surprise bills.

Pharmacy Benefit Manager
You get access to our negotiated pass-through pricing contract through Express Scripts for significant savings due to steep discounts and higher rebates than other pricing models. We also have the flexibility to work with other PBMs if your group prefers.

COBRA Administration
We administer COBRA continuation of coverage at no additional cost for the lines of business covered by EMI Health (medical, dental, and/or vision). Each person on COBRA will be charged 102 percent of the active employee rate.

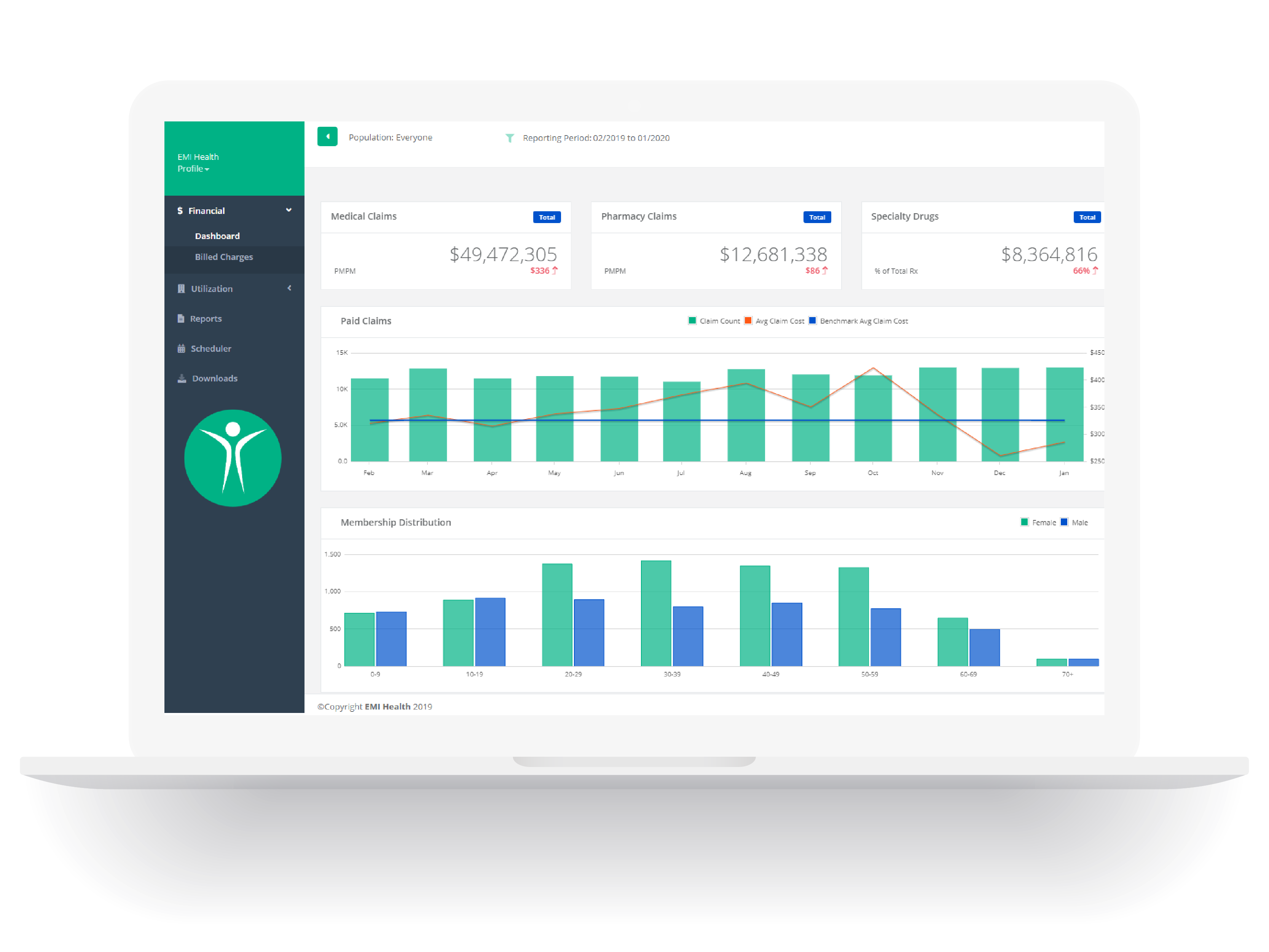
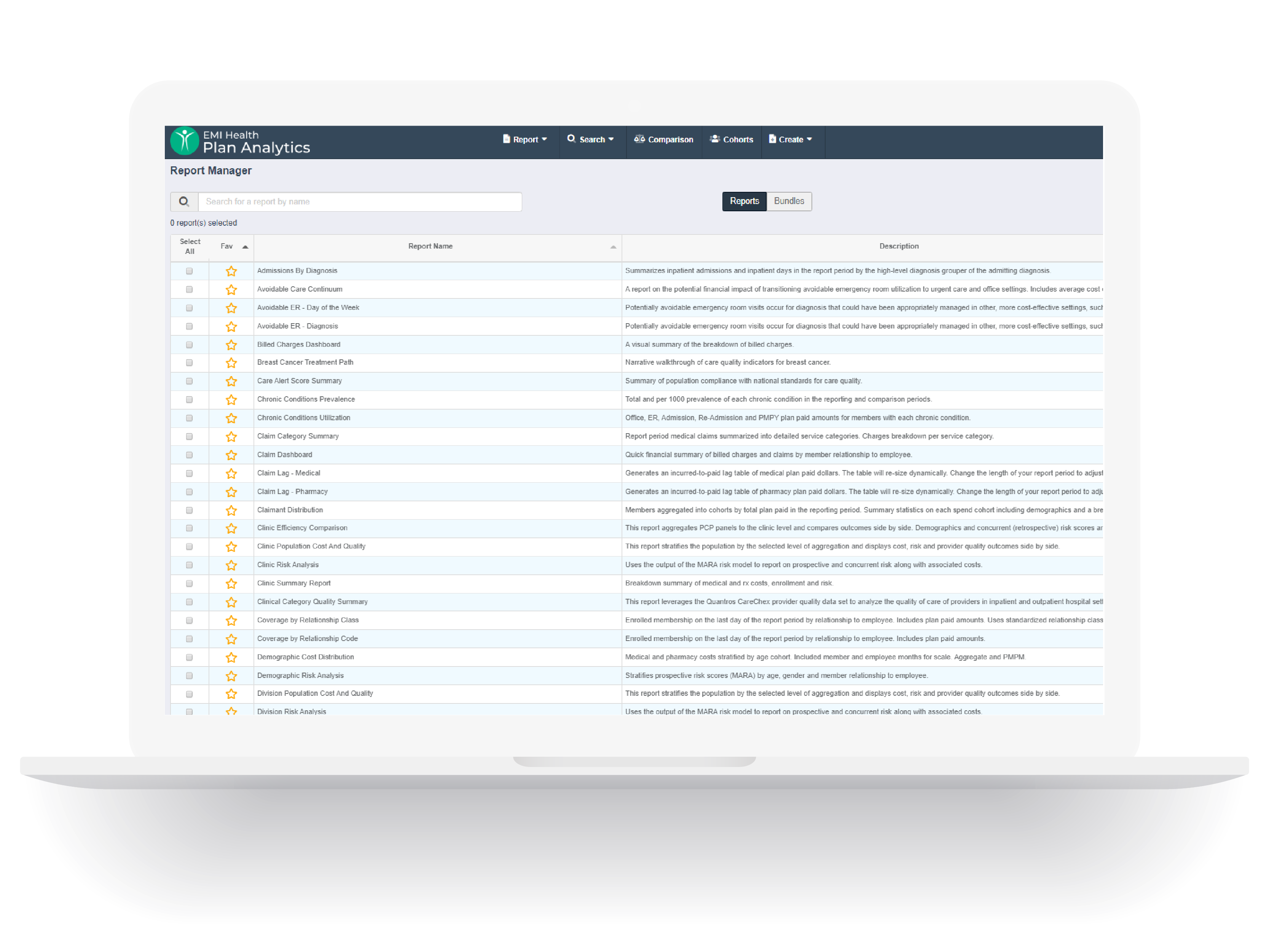
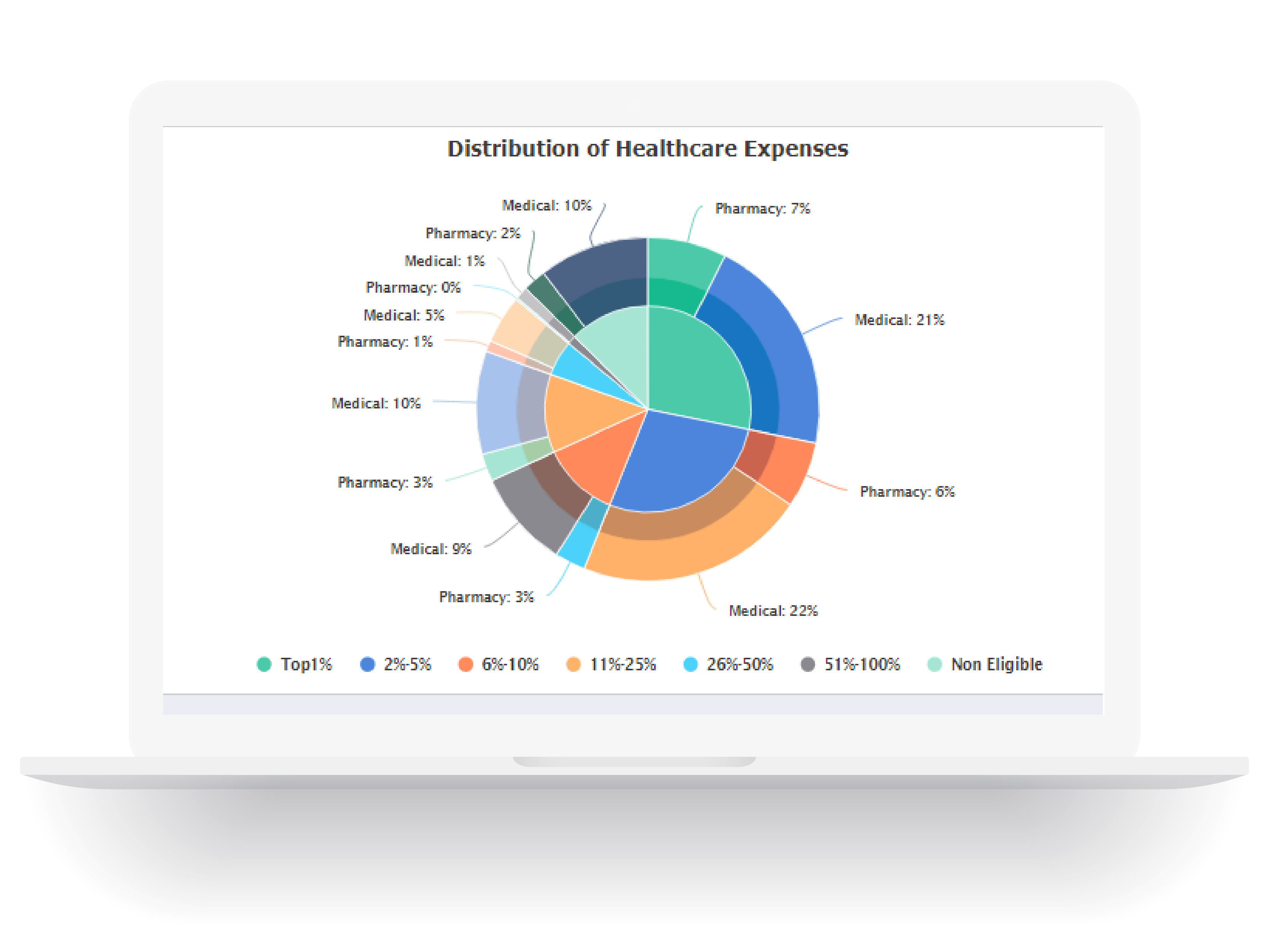
Reporting
Capability
We have in-house capability to run numerous reports, and we accommodate non-standard reporting requests whenever we can. Know where your claims dollars are going, and get guidance on what can help your plan perform better year after year.